In the increasingly complex American healthcare system, getting insurance coverage is only half the battle for plan members.
Accessing that care in a cost-effective and informed way is another matter entirely.
According to a 2023 KFF report, a majority of insured adults (58%) say they have experienced problems using their health insurance, such as denied claims, provider network problems, and pre-authorization problems. Among those members, 17% say they were ultimately unable to receive the care they needed, with about 15% experiencing a subsequent decline in their health.
To combat this frustration and the ever-rising costs of American healthcare, health benefits plans and the payers who sponsor them must embrace innovative, member-centered tools — most notably, healthcare navigation solutions.
In this guide, we’ll explore what those solutions look like, how they support value-based care and cost containment, and how Vālenz Health® is leading the industry with care navigation tools that engage across the entire member journey to deliver smarter, better, faster healthcare for all.
Table of Contents
- Healthcare Navigation: What it is and How it Works
- Why Healthcare Navigation Matters
- The Importance of Independent Healthcare Navigation Tools
- How Vālenz Health® Care Navigation Tools Create Smarter, Better, Faster Healthcare
Healthcare Navigation: What It is and How It Works
In the simplest terms, healthcare navigation is a strategy through which members can more directly and effectively manage their personal care journeys using resources such as cost and quality transparency and care coordination.
Healthcare navigation solutions put the power in the members’ hands, allowing them to make informed decisions about their healthcare and alleviating the complexity of the modern health system through:
- Provider network directories that identify and list in-network providers and facilities
- Cost and quality transparency tools that include objective care quality rankings and estimated member out-of-pocket costs
- Pharmacy benefits tools that identify and recommend clinically comparable, lower-cost alternatives to high-cost prescriptions
- Care navigation services that provide personalized support to members in need of complex or high-cost procedures
Typically, care navigation services are provided digitally, allowing plan members to evaluate their care options through online platforms and directories. Members can also contact care navigators via phone to receive assistance when scheduling appointments, transferring medical records, and creating a care management plan for their needs.
Why Healthcare Navigation Matters: Benefits for Patients, Payers, and Plans
By helping members understand the cost and quality of providers before they schedule care, healthcare navigation tools are instrumental in bettering health outcomes, reducing costs, and improving employee engagement in their personal healthcare journeys.
When members are empowered with information about their care choices, they no longer feel at the mercy of the complex American healthcare system. Instead, they are given the power to choose the right care at the right time (and at the right price) for their personal needs — a choice that bolsters their patient experience and satisfaction levels.
With this focus on personalized, informed decision making, healthcare navigation tools play an instrumental role in the advancement of a value-based care system. By directing patients to low-cost, high-value healthcare providers and facilities, care navigation solutions are expected to be a cornerstone feature in health plans of the future, thanks to their potential for cost containment, better care outcomes, and more.
Informed Decision Making
In 2023, more than one-third of all insured adults said it was “somewhat” or “very difficult” to understand what their insurance will and will not cover. At the same time, 58% of Americans say they would be willing to shop for their care choices if pricing information was disclosed beforehand.
Healthcare navigation services work to fill that gap, providing the transparency needed for members to make care choices based on pricing and care quality data.
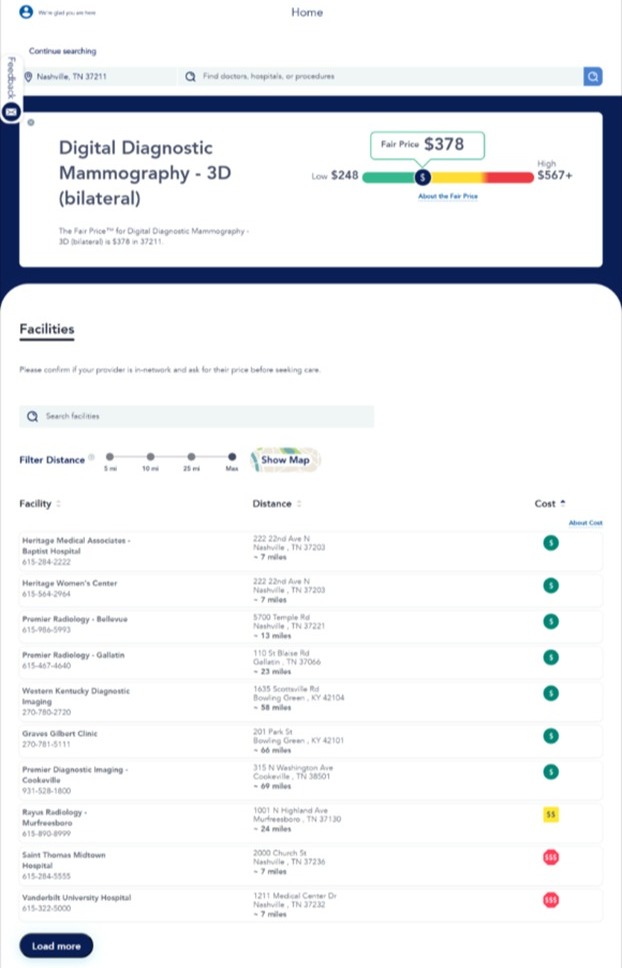
Detailed, accurate cost and quality transparency tools help members find in-network providers who perform common shoppable procedures, allowing them to sort by estimated out-of-pocket costs, care quality rankings, travel distance, and other important factors.
Where those digital, self-service tools fall short, care navigators can step in with the personalized education members deserve. Plan members who connect with care navigators can get answers to their specific care questions, as well as receive personalized care management support to guide them through their unique healthcare experience.
Reduced Healthcare Costs
Many members fail to realize just how wildly procedure costs can vary based on insurance plans, providers, and facilities used. As just one example, the median cost of a diagnostic colonoscopy can range from $925 to $3,571, according to a recent JAMA study.
 Source: JAMA Network Open.
Source: JAMA Network Open.
With healthcare navigation solutions, members are made aware of these costs before scheduling care, empowering them to select more affordable options that reduce overall healthcare spend for themselves and their employers.
For example, employers who offer Valenz Bluebook in their benefits package save an average of $1,500 every time a member uses the tool. The color-coded, “green-yellow-red" analysis helps members find low-cost, high-value providers — those “green” providers who administer care at what we call a Fair Price™ — while simultaneously identifying those who charge higher prices than market value.
Care navigation can also be instrumental in reducing rising pharmaceutical costs. Pharmacy benefits solutions such as Integrated Health Management (a featured of Valenz Bluebook Rx) create fixed drug costs while improving access to essential medications through data-driven market analysis, strategic coupon use, and more — lowering member and employer pharmacy expenses, as evidenced by the 70% savings in specialty drug costs experienced by one Valenz client.
To reduce the costs of expensive, complex surgical procedures, plan payers can also employ direct contracting networks. By combining these networks with intuitive care navigation, employers can help guide members to the right care options at the right price — and, in the case of Valenz Precision Care, deliver 50% or more in savings on certain procedures.
With healthcare price increases continuing to outpace general inflation rates, care navigation tools hold great potential for minimizing member costs, especially when the cost to access that care in the first place (premiums) is expected to rise significantly in 2026.
In addition, by emphasizing a value-based approach that prioritizes low-cost and high-value care options, care navigation tools will not only help to reduce today’s healthcare costs but also minimize future expenses with a preventive care strategy — one that improves long-term member outcomes.
Improved Care Outcomes
When members delay or avoid necessary care because of the complexities involved, the effects are long-lasting. Those who reported delaying care during the COVID-19 pandemic were more likely to have chronic illnesses, conditions which can lead to serious long-term effects when left untreated.
Even with no major pandemic restricting care, not all plan members have equal access to the high-quality healthcare they deserve. Members of vulnerable socioeconomic groups — including Black, Hispanic, American Indian and Alaska Native, and Asian American, Native Hawaiian, and Pacific Islander populations — experience significant health disparities in the U.S. Many are less likely to have a usual source of care or regularly receive timely preventive services, which contribute to higher rates of serious health conditions.
Healthcare navigation tools help resolve these access challenges by meeting members where they are, educating them about their care options, and connecting them to the right services for their needs.
Solutions like care navigators have been proven to improve outcomes for underserved populations, addressing issues related to provider distrust and empowering vulnerable communities to take charge of their personal healthcare journeys. And the effects aren’t limited to certain socioeconomic groups; care navigation solutions have also improved preventive care uptake (in the form of cancer screenings) and health-related quality of life scores for elderly patients.
Better Healthcare Experience
The American healthcare system has a reputation of confusing members, especially when only 12% of adults are considered “proficient” in terms of healthcare literacy. Navigation solutions help level the playing field, in turn improving the entire healthcare experience for plan members.
With access to solutions like care concierges, who guide members through the complicated healthcare ecosystem to find high-quality care, patients are no longer left to navigate the system on their own. When members are provided expert support with complicated processes such as scheduling, medical record transfer, and billing review, they’re less likely to put off needed care — and may be more likely to report higher levels of satisfaction with their care journeys.
The Importance of Independent Healthcare Navigation Tools
While most healthcare navigation tools provide the benefits listed above, they’re not all created equally. To maximize the cost and time savings for both members and employers, health plans should prioritize independent navigation tools over those provided by specific carriers.
The difference is in the data that drives them both.
Most carrier-sponsored tools are powered by information based on negotiated rates between plans and providers, rather than actual medical claims. The wealth of data is often limited to the plan’s internally reported information, which can include self-reported quality data with a degree of bias.
This lack of data can severely limit the effectiveness of carrier-specific healthcare navigation tools. Price and quality databases can be incomplete or inaccurate, and care navigators may not have the full knowledge of which low-cost, high-value options are available to members.
Independent tools, such as those provided by Valenz, take a more comprehensive, objective approach — one in which members are directed to the absolute best option for their needs, regardless of carrier or network affiliations.
By incorporating medical quality, clinical performance, and pricing data from a wealth of objective, independent sources, Valenz provides a comprehensive, data-driven approach to healthcare navigation tools. Tools like Valenz Bluebook are fed by unbiased data sources, empowering members to make informed decisions without the obligations set by certain carrier networks.
To learn more about our data-driven approach to healthcare navigation solutions, contact our team today.
How Vālenz Health® Care Navigation Tools Create Smarter, Better, Faster Healthcare
Recognizing the importance that navigation solutions play in an increasingly complex and expensive healthcare ecosystem, Valenz has long established itself as the leader in providing data-backed, member-focused tools that improve the entire patient journey.
Through our suite of Member Experience solutions, we provide intuitive navigation that empowers members to find the right care at the right time, ultimately delivering improved clinical care and better health outcomes with:
- Valenz Bluebook: Our cost and quality data transparency solution (compliant with TiC and No Surprises Act regulations) allows members to search by provider, facility, or procedure to compare information and find the best care for their needs.
- Valenz Bluebook Rx: Our pharmacy benefits management solution combines data-driven insights with member engagement tools to minimize prescription drug costs for patients and payers.
- Valenz Clinical Engagement: Our comprehensive suite of care management services guides members to the most appropriate levels of care from the start of their health journeys, empowering better decision-making and reducing unnecessary healthcare utilization.
- Valenz Precision Care: Our personalized navigation and high-value care solutions for complex procedures connect members to convenient, high-quality care tailored to their needs, proactively identifying and recommending cost-savings opportunities using member-specific data.
By engaging early and often with plan members, the Valenz care navigation solutions enhance decision-making at every step of the care journey, delivering higher cost savings and health outcomes through personalized member engagement strategies.
To see what a tailored strategy could look like for your health plan — and what kind of results care navigation could create for you — contact a Valenz team member below.

